Osteochondrosis of the cervical spine is a pathological condition in which degenerative changes occur in bone and cartilaginous tissue.
Dystrophy of the intervertebral discs can develop after the age of 30, while at the age of 40-45 they become dry and hardened.
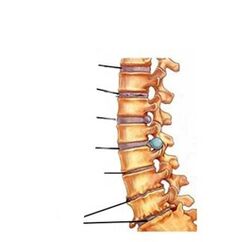
The spinal column contains 7 cervical vertebrae, consisting of a body, processes and a bony arch;In the center of the vertebra there is a hole where the spinal cord is located.The individual elements of the spinal column are connected to each other by intervertebral discs formed by a nucleus, a fibrous ring and a layer: the hyaline plate (cartilage).The cervical vertebrae, having the smallest thickness of the discs, adapt perfectly to each other;the muscles in the neck area are rather poorly developed, so with regular exercise, disc displacement may occur, which compresses blood vessels and nerve trunks.
The disease goes through several stages in its development, during which the spine undergoes pathological changes:
1st degree osteochondrosis
Characterized by the onset of destruction of the intervertebral discs.Cracks form in the fibrous ring, the strength and elasticity of the disc are impaired, its height decreases, due to which the nerve roots are compressed.A characteristic aching pain appears.Sometimes in stage 1 (preclinical) such pain may be absent, and osteochondrosis is manifested by moderate discomfort in the neck area.
2nd degree osteochondrosis
If grade 1 osteochondrosis was not treated or the treatment was not effective, a chronic condition occurs, which is grade 2 osteochondrosis. The pain becomes constant, the destruction and compaction of the intervertebral disc continues and leads to mild dislocations of the cervical vertebrae.With cervical osteochondrosis, drooping head syndrome may develop at this stage.This syndrome is characterized by severe pain and the person is forced to support the head in a fixed position to reduce the pain.
3rd degree osteochondrosis
The fibrous ring is almost destroyed, which leads to complications of osteochondrosis: protrusion (impingement) of the intervertebral disc or intervertebral hernia.At stage 3 of osteochondrosis, the intensity of pain may decrease, since the affected cartilaginous tissue in the intervertebral disc simply no longer exists, and therefore there is no source of pain, however, pinching of the nerve roots remains, so the pain does not disappear completely.
Causes of cervical osteochondrosis
With age the nucleus of the intervertebral disc loses its moisture reserves and also becomes less elastic.Since the metabolism slows down significantly after 50 years, the regeneration processes in discs with poor blood supply stop.At a young age, the main role in the onset of osteochondrosis in the cervical spine is played by physical inactivity: a passive lifestyle, lack of properly organized physical activity.
Factors that contribute to poor circulation in the cervical vertebrae and intervertebral space are:
- drive a car for a long time;
- working at a computer, sitting for long periods of time in any position;
- regular weight lifting;
- working conditions involving sudden movements and rotations of the neck;
- bad posture;
- neck and head injuries;
- displacement of the disc following sports training;
- excess weight, which leads to a high load on the intervertebral discs and disruption of the functioning of the cervicothoracic spine;
- alcohol abuse, smoking, poor diet (due to harmful effects on metabolic processes);stress;
- hypothermia of the neck (for example, in the absence of a scarf during the cold period);
- sleeping on high or too soft pillows;
- heredity (family history of spinal diseases).
Common symptoms of neck osteochondrosis may include:
- dizziness, migraine-like pain in the head (sharp), as well as dull, pressing pain in the neck (cervicalgia), which may intensify when you move your head;
- low back pain (sharp pain that spreads to the back or arm);
- burning pain in the back, heart;
- stiffness of the neck, arms (especially the hands);
- decreased mobility and numbness in the neck in the morning;
- throbbing sensation in the back of the head;
- temporary darkness in the eyes, noise in the ear canal, sometimes fainting;
- thickening of the skin in the spine due to proliferation of connective tissue.
Diagnostics
Most often, the doctor's diagnosis sounds like "cervical osteochondrosis of the 2nd degree".Why immediately the second?The fact is that the first degree cannot be diagnosed because the symptoms are too weak.During a preliminary examination, the doctor determines how damaged the spine is.For this, the patient is examined in different positions: horizontal, sitting, standing, inclined.Counting the vertebrae, the specialist focuses on anatomical norms and determines the degree of osteochondrosis of the cervical spine.The examination is not limited to a visual examination: the spinal deformity can be easily palpated with the hand.Palpation allows you to determine the localization of pain and the strength of tension in the paravertebral muscles.However, in order for the treatment of osteochondrosis of the cervical spine to give positive results, it is necessary to undergo a hardware examination.Computed tomography, x-ray, magnetic resonance imaging - all these methods make the diagnosis perfectly accurate and allow you to choose the optimal treatment method.
Treatment
How to cure osteochondrosis of the cervical spine?This is the wrong way to ask the question;more correctly, how to treat osteochondrosis of the cervical spine, since it is completely impossible to cure osteochondrosis.But it is quite possible to stop the process of destruction of cartilaginous tissue and intervertebral discs and eliminate pain and discomfort.But this is only possible if treatment is started at an early stage of the disease.Therefore, it is so important to consult a doctor in a timely manner.
Treatment of osteochondrosis of the cervical spine should be comprehensive.
The treatment regimen can be presented as follows:
- drugs from the NSAID group (non-steroidal anti-inflammatory drugs) to relieve inflammation;
- antispasmodics: to relieve spasms;
- painkillers;
- B vitamins;
- reflexology;
- physical therapy (physical therapy) - eliminates pain and inflammation;
- therapeutic massage: restores blood supply, relieves tension;
- acupuncture and acupressure.
But the most important method of treating cervical osteochondrosis is dosed physical activity.
Disease prevention
To prevent the development of cervical osteochondrosis, it is recommended:
- when working in a sedentary manner, be sure to take five-minute breaks every hour, avoid strain on the neck,
- do not make sudden head movements, pay attention to your posture,
- avoid hypothermia,
- do physical activity, swim, eat well,
- sleep should take place on a firm mattress and a low pillow: the bending angle of the neck should not be more than 15 degrees,
- after 25 years, avoid shock loads on the spine (jumping, running).

















